Seniors and people with disabilities are often more isolated and at heightened risk for malnutrition. Since COVID-19 ushered in an era of limited contact, that danger has increased. And it’s something healthcare foodservice providers and those who work in community-based services can address.
A national poll by the University of Michigan shows loneliness has more than doubled among older adults during the first few months of COVID-19. This raises the risk of malnutrition, which typically increases with social isolation and loneliness, resulting in these negative impacts:
- Reduced enjoyment of food
- Loss of appetite, reducing the number of meals eaten daily
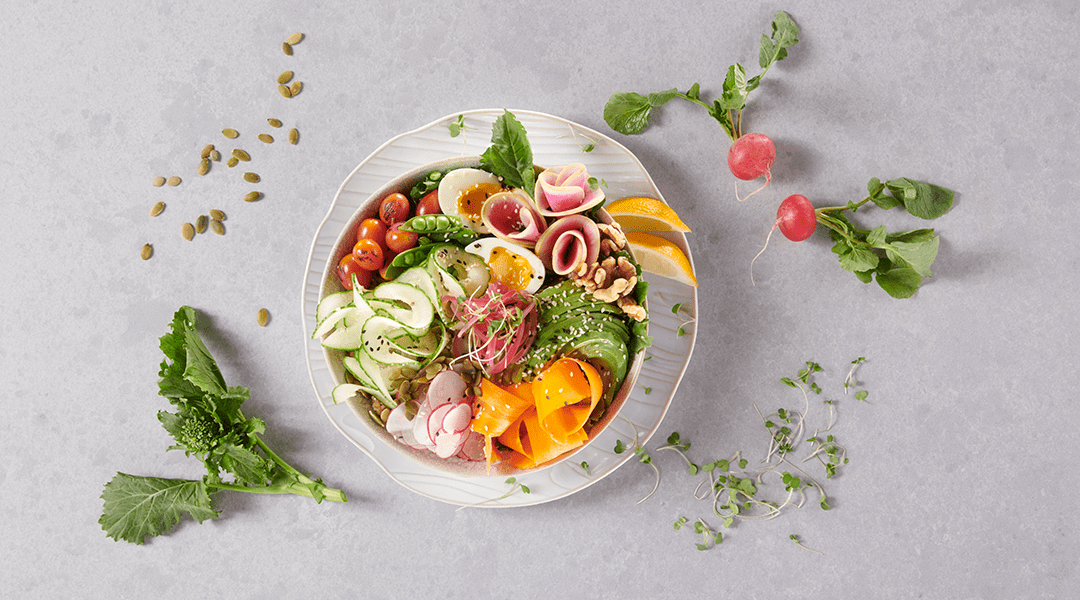
- Diminished diet quality, with a lower intake of protein, fruits and vegetables
The picture is expected to get worse before the end of the year. According to The State of Food Security and Nutrition in the World, 2020, the pandemic could add 83 million to 132 million people to the undernourished category.
What can you do about it?
Helping seniors eat better requires working with them across the continuum of care, especially when discharging them from an inpatient setting. Make sure to address these five categories:
Groceries. People need to be able to eat well after discharge.
- Ask whether they will have enough groceries when they get home.
- Ask who does the shopping and provide guidance.
- Make sure expired/spoiled foods in the fridge are discarded.
Meal preparation. Having the right food is only the first step.
- Can they prepare their own meals?
- If not, has help been arranged—a loved one or home meal delivery—until they are able?
Diet recommendations. The food they once ate may not be best for nutrition and/or recovery.
- Does their food need therapeutic or consistency modifications?
- Do they need training on a new diet?
- Does this affect grocery shopping and/or meal preparation?
Adaptive equipment. Make eating easy and appetizing.
- Do they need special seats, trays, plates, utensils or drinkware to consume food?
- Do they know these items exist and where to get them? Help with referrals.
Food insecurity. Often associated with poverty, this can affect anyone.
- Do they have access to food (especially important during this pandemic)?
- Explain about community food programs, such as Meals on Wheels.
- If a program is unavailable consider starting a meals-to-go program of your own.