Few things are as pleasing to the senses as the warmth and aroma of fresh-baked bread. That kind of feel-good therapy is exactly what the Mid-Michigan Medical Center-Gladwin tries to achieve by sending each one of its patients home with warm, aromatic loaf of artisan bread.
The goal of giving discharged patients a loaf of cranberry walnut bread or Italian bread was to say thanks, getting patients to think to themselves, “Hey, I didn’t expect that from a healthcare provider,” says Julie Reid, Nursing Campus Manager in Gladwin.
She and her staff hoped the simple gift of bread could improve patient response scorecards as a token of appreciation for choosing MidMichigan Medical Center. But a funny thing happened on the way from the oven to the patient’s bedside—it opened a door to a conversation.
“It helped get us in the room and talking with patients, Reid says. “It let them know we care about their health not only while they’re here, but after they leave.”
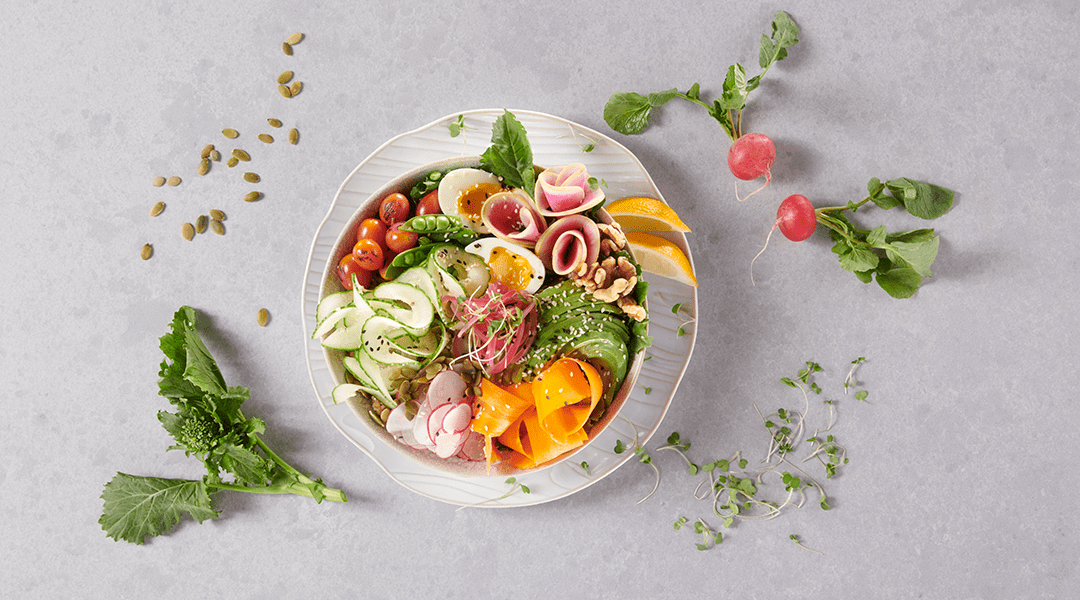
That simple loaf of bread opens the door to recognizing how important eating and nutrition are to continuing health. Research has shown that people who are hospitalized lose their appetite and consume less food—all at a time when they need nutrients to boost their immune system to help them heal.
Discharge planning takes a closer look at nutrition therapy
Once they leave the hospital, patients are unlikely to stop at the grocery store and buy healthy foods. It’s easy to see how this can lead to overlooking good nutrition and its importance on health, wellness, and strength. And former patients who struggle to thrive are more likely to be readmitted to the hospital.
“A loaf of bread is not a magic bullet that solves all of the eating and nutrition concerns,” says Dana Fillmore, RD, Gordon Food Service U.S. National Healthcare Marketing Manager. “What it provides is food that is warm, inviting, and ready to consume—something that increases your interest in eating.”
With surveys that show a third of hospitalized patients are malnourished upon admission, care centers have made nutrition not only a treatment priority, but also a key part of discharge planning.
In fact, the Centers for Medicare & Medicaid Services published proposed rules to improve the discharge planning requirements that certain hospitals, post-acute care providers, and home-health agencies must meet to participate in the Medicare and Medicaid programs. The rule focuses on patient preference. One key component that must be included in discharge planning is communication about specific nutrition needs when a patient transitions out of the hospital and back home, to rehab, to a long-term care center, etc.
“If you send patients home with the names of agencies they can contact for help, there is no guarantee they will follow through,” Fillmore says. “If you send them home with the right ingredients to get them thinking about eating and nutrition, you’re on a better path toward reducing readmission.”
In 2014, Lee Memorial Hospital in Florida tested a medical nutrition therapy program that addresses food needs for discharged patients. Called Flavor Harvest, the program delivers prepared, individually packaged food once a week for four weeks (28 days) after discharge. This includes three meals a day, plus snacks, liquid supplements ordered by the patient’s doctor, and counseling by a dietitian. Of 101 patients informed about the program, 59 received all meals and the readmission rate was 17 percent. Of the 42 who did not receive meals, 28 percent were readmitted.
Begin with small, affordable and patient-pleasing foods
“It takes a lot of planning, organization, and funding to do what Lee Memorial did,” Fillmore says. “The idea of offering a loaf of bread is a manageable and affordable way to start.”
To make going home less stressful, Western Reserve Hospital in Cuyahoga Falls, Ohio, sends a quart of homemade chicken noodle soup home with people who have undergone outpatient procedures.
“For some discharged patients, standing up and preparing food in their kitchen just isn’t a priority, so soup or a loaf of bread is a reminder that eating and nutrition is important,” Fillmore says. “If a relative or family member is there at the time of discharge, it’s an opportunity to share the message about the importance of stimulating the patient’s appetite.”
Patients at MidMichigan have been very appreciative of the loaves of bread, Reid says, and its possible the program could be expanded. She said offering fruits and vegetables, gift cards to markets, or simple recipe ideas have been suggested.
The Gordon Food Service Nutrition Resource Center has dietitians on staff and nutrition information available for all of our products so you can make food and nutrition a healthy part of your discharge program. Whether you choose to provide a complete meal program or a hearth-baked loaf of bread, it could be just what the doctor ordered.