When it comes to improving the dining experience in senior living, operators often focus on overall atmosphere, menu quality, and waitstaff service. All too often, those efforts can be quickly diminished by disruptive diners. Cliques, messy eaters, and other disruptive diners can be a common concern in independent- and assisted-living environments.
That means it’s imperative for dining services to spot and defuse situations that threaten mealtime serenity.
Mealtime is residents’ “social time—their time to get around their friends and neighbors,” says Brenda Berning, Culinary Services Director at Luther Oaks in Bloomington, Illinois. Luther Oaks is a community of independent-living apartments and assisted-living apartments, some with memory-support services. Berning’s goal: To promote a relaxed, comfortable setting at mealtimes.
Become a clique buster
One disruption comes in the form of cliques—groups of diners who exclude others. Have staff keep an eye out for signs of cliques, for instance residents approaching, then leaving a table without sitting down, or eating quickly and leaving without finishing their meal. If certain residents stop eating, or seem not to enjoy meal periods, ask questions to help uncover clique-ish behavior. Broach the subject delicately; you may have to do it more than once as some residents may feel embarrassed or reluctant to talk.
Open seating can empower cliques, says Carmen Bowman, owner of Edu-Catering, a Denver-area consulting firm focusing on culture change. Friends will arrive at dinner early, save a table, then shoo away others who try to sit there.
Assigned seating is an option, though residents might resist, claiming that they have rights, Bowman says. Her solution: Initiate a discussion. “‘We have a problem here,’” Bowman suggests by way of conversation. “‘People aren’t being treated right … People are feeling bad. How do we solve that together?’”
Encourage neater eaters
Messy eaters can ruin meals for other diners. “It is a very difficult situation,” says Corinne Inchauste, Certified Dietary Manager at Spectrum Health Rehab and Nursing Center in Grand Rapids, Michigan. “People say, “I’m not sitting with her; she’s messy.’”
Bowman points out that proper equipment—tremor-canceling flatware, weighted coffee mugs half-filled, and white plates that make it easier for residents to see the food—help reduce mess at mealtimes.
Cutting food into bite-size pieces helps, as does turning dinner into finger foods. Bowman recommends Dining with Friends, a video produced by the Alzheimer’s Resource Center and available for free on its website, arc-ct.org.
Peace and quiet can prevail
To calm disruptive diners, Bowman suggests enlisting the entire staff. Endeavor to make every meal “the best dining experience ever for these people,” she says. Serving appetizers, letting diners know how long it will be until entrées are served, and overall making them comfortable can alleviate most disruptions.
Fashioning the dining room into smaller, more intimate spaces with plants or room dividers can also help. “You get lost in a big room with other people,” Bowman points out. Smaller dining areas are also easier for staff to control.
Bowman recommends having staff sit with guests during meals to keep the conversation running. One idea: Keep residents’ pertinent info—their career, where they grew up, how many children and grandchildren they have—on index cards. During meals, refer to the cards to create conversations.
Rising to the occasion
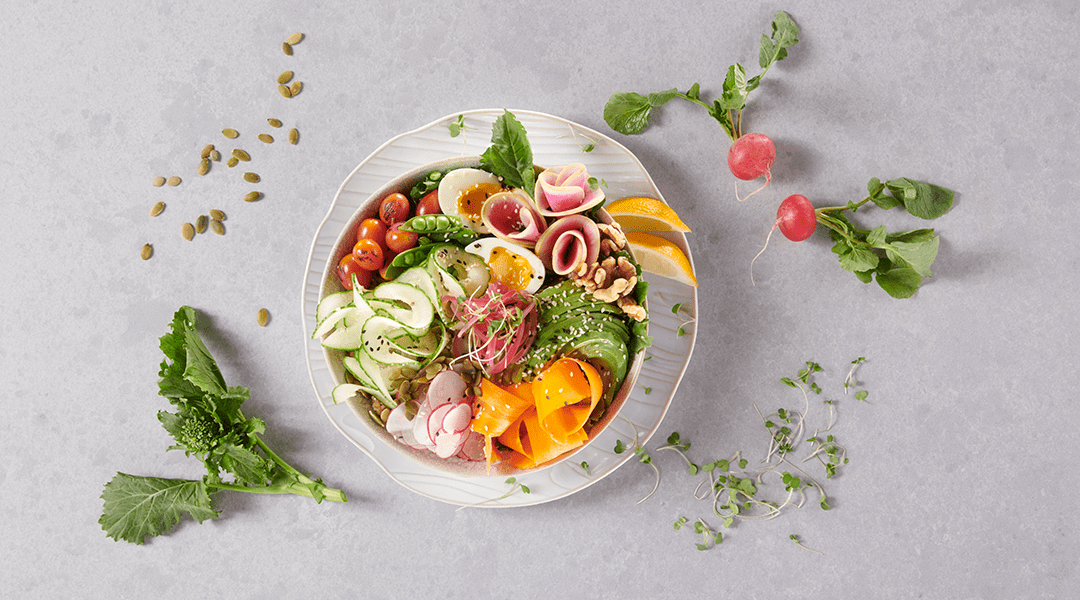
A final suggestion: Make the dining room lovely to inspire good behavior. Cover tables with tablecloths. Use cloth napkins and real china and tableware. White plates make food more visible, more accessible to sensory-impaired residents, and better display beautifully prepared and plated foods.
The point of culture change, Bowman stresses, is a move toward a resident-centric culture that closely mirrors settings residents enjoyed before life and their age intervened. “We have to be more proactive with life and care and service to people who live in institutions,” Bowman says.
The Legal Side of Dining Dynamics
The Fair Housing Act and the Americans with Disabilities Act govern what may be done to solve dining-room issues, says Scott Moore, an attorney and partner at Baird Holm in Omaha, Nebraska.
Broadly speaking, the Fair Housing Act applies to independent-living facilities. Americans with Disabilities Act (ADA) regulations apply to assisted-living facilities and those with a higher level of care. In cases where residents from an independent-living home and assisted-living home share a dining room, both Fair Housing and ADA apply. Both sets of regulations are “pretty consistent on what you can and cannot do,” Moore says.
Regulations consider whether a person’s actions threaten or disrupt the peace and enjoyment of others. If that’s the case, institutions can act and, say, remove that person from the dining area. The person, however, has to be truly disruptive—yelling and throwing things, for instance. “You can’t exclude someone because people are uncomfortable,” Moore says.